Understanding a Normal Sperm Analysis Report (PDF)
Semen analysis‚ often in PDF format‚ is crucial for evaluating male fertility; the 6th Edition details advanced testing like SDF‚ aiding comprehensive assessment.

Semen analysis is a cornerstone in the evaluation of male fertility‚ providing critical insights into a man’s reproductive potential. Typically delivered as a PDF report‚ this test assesses various characteristics of semen and sperm. The 6th Edition of relevant guidelines emphasizes its importance‚ acknowledging emerging biomarkers like Sperm DNA Fragmentation (SDF) as valuable additions to the standard workup.
Understanding the nuances of a semen analysis report is vital for both clinicians and patients. It’s not merely about a single number‚ but a holistic evaluation of volume‚ concentration‚ motility‚ and morphology. The report helps identify potential issues impacting natural conception and guides appropriate therapeutic interventions. Age-related changes in semen parameters are also considered‚ with reference ranges evolving to reflect these shifts.

Key Parameters Assessed in a Sperm Analysis
Semen analysis‚ often a PDF‚ meticulously evaluates volume‚ concentration‚ motility‚ and morphology—key indicators of sperm quality and male fertility potential.
Semen Volume
Semen volume‚ typically reported in milliliters (ml) on a PDF sperm analysis report‚ represents the total fluid ejaculated. The 6th Edition of andrology guidelines acknowledges semen volume as a foundational parameter. Normal values generally range‚ but recent analyses demonstrate a trend; studies show a mean decrease from 3.79 ml to 3.42 ml (p < 0.05) over time.
Low semen volume could indicate issues with seminal vesicle function or a blockage. Conversely‚ high volume doesn’t necessarily equate to better fertility. The 5th centile is used as a reference‚ but laboratory-specific ranges‚ detailed within the PDF report‚ are vital for accurate interpretation. Assessing volume is a crucial first step in evaluating male factor infertility.
Sperm Concentration (Sperm Count)
Sperm concentration‚ measured in millions of sperm per milliliter (mill/ml) and detailed in a PDF report‚ is a key indicator of male fertility potential. The 6th Edition emphasizes its importance. Recent data reveals a significant decline; the mean sperm count decreased from 125.4 mill/ml to 78.0 mill/ml (p < 0.001) over a studied period.

A low sperm count can stem from various factors‚ including hormonal imbalances or testicular issues. The 5th centile serves as a benchmark‚ but individual laboratory reference ranges‚ found within the PDF‚ are essential for precise evaluation. Understanding these values‚ alongside other parameters‚ helps determine appropriate diagnostic and therapeutic interventions for male infertility.
Total Sperm Number
Total Sperm Number (TSN)‚ often reported within a PDF semen analysis‚ represents the overall sperm count – concentration multiplied by semen volume. While concentration indicates sperm density‚ TSN provides a more comprehensive assessment of a man’s fertilizing capacity. The 6th Edition acknowledges its significance alongside other parameters.
A declining trend in TSN is noted; studies show a decrease from 125.4 million to 78.0 million (p < 0.001). This parameter‚ detailed in the PDF report‚ is crucial because a sufficient TSN is necessary for successful fertilization. Laboratories establish reference ranges‚ and abnormal TSN values warrant referral to a male reproductive specialist for further evaluation and potential treatment.
Sperm Motility
Sperm motility‚ a key component of a PDF semen analysis report‚ assesses the sperm’s ability to move effectively. It’s categorized into progressive and non-progressive motion‚ impacting fertilization potential. The 6th Edition emphasizes motility as a critical factor in male fertility assessment.
Progressive motility – forward‚ straight-line swimming – is particularly important. A PDF report will detail percentages for each motility type. While the 5th centile values are a guide‚ interpreting motility requires considering the entire semen profile. Abnormal motility‚ as documented in the PDF‚ often prompts referral to a specialist for comprehensive evaluation and potential intervention.
Progressive Motility
Progressive motility‚ detailed within a PDF semen analysis report‚ signifies sperm swimming actively in a straight line‚ vital for reaching and fertilizing the egg. The 6th Edition highlights its importance in evaluating male fertility potential. A PDF will quantify the percentage of sperm exhibiting this forward progression.
This parameter is crucial because it directly correlates with fertilization capability. Lower percentages‚ as indicated in the PDF‚ may suggest difficulties in natural conception. Reference ranges‚ often lab-specific as noted in the PDF‚ help determine normalcy. Abnormal progressive motility often necessitates further investigation by a male reproductive specialist‚ as outlined in comprehensive reports.
Non-Progressive Motility
Non-progressive motility‚ reported in a PDF semen analysis‚ describes sperm movement that is slow‚ sluggish‚ or in large circles – lacking the forward trajectory needed for fertilization. The 6th Edition acknowledges its role in a complete assessment of sperm function. A PDF report will detail the percentage of sperm displaying this type of movement.
While not as indicative of fertility as progressive motility‚ a high percentage of non-progressive sperm‚ as shown in the PDF‚ can still contribute to infertility. It suggests potential issues with sperm energy or structural integrity. Lab-specific reference ranges within the PDF are vital for interpretation‚ and abnormal results warrant specialist evaluation.
Sperm Morphology
Sperm morphology‚ detailed in a PDF semen analysis report‚ assesses the shape and structure of individual sperm cells. The 6th Edition emphasizes its importance alongside motility and concentration. A PDF will present the percentage of sperm with a normal shape‚ crucial for penetrating the egg. Abnormal morphology‚ categorized by head‚ midpiece‚ or tail defects‚ is also reported.
The PDF report utilizes strict criteria (Kruger’s) to classify these defects. Increased abnormal forms‚ as noted in the PDF‚ can hinder fertilization. Age-related changes‚ with a noted increase in double sperm heads‚ are also documented. Reference ranges within the PDF‚ alongside specialist interpretation‚ are essential for accurate assessment.
Normal Morphology
A normal sperm morphology report‚ detailed within a PDF semen analysis‚ signifies sperm possessing the ideal shape for successful fertilization. The 6th Edition highlights the importance of Kruger’s strict criteria for assessment‚ as presented in the PDF. This includes a properly formed head‚ midpiece‚ and tail‚ enabling effective movement and egg penetration.
The PDF report will indicate the percentage of sperm exhibiting this normal form. While the 5th centile is a benchmark‚ laboratory-specific reference ranges within the PDF are vital for interpretation. A higher percentage of normally shaped sperm correlates with improved fertility potential‚ as detailed in the PDF’s findings.
Abnormal Morphology (Head‚ Midpiece‚ Tail Defects)
A PDF semen analysis report detailing abnormal morphology identifies sperm with defects in the head‚ midpiece‚ or tail. The 6th Edition emphasizes detailed categorization of these abnormalities. Head defects might include a small‚ large‚ or tapered shape‚ impacting egg penetration. Midpiece issues‚ as noted in the PDF‚ can affect sperm motility. Tail defects hinder progressive movement.
The PDF report quantifies the percentage of sperm exhibiting these flaws; Increased levels of abnormal forms‚ exceeding laboratory-defined thresholds within the PDF‚ can indicate reduced fertility. The PDF’s reference ranges‚ crucial for interpretation‚ help determine the clinical significance of these morphological abnormalities‚ potentially prompting further evaluation;

Advanced Semen Analysis Tests
PDF reports increasingly include tests like Sperm DNA Fragmentation (SDF) and Reactive Oxygen Species (ROS) assessment‚ offering deeper insights into sperm quality.
Sperm DNA Fragmentation (SDF)
Sperm DNA Fragmentation (SDF) testing‚ detailed within PDF semen analysis reports‚ is gaining prominence as a vital biomarker for male infertility evaluation. The 6th Edition acknowledges SDF’s importance‚ linking DNA integrity to successful embryo development‚ implantation‚ and overall pregnancy rates. Several methods are employed‚ including the TUNEL assay and the Sperm Chromatin Dispersion Assay‚ both deemed useful for clinical application‚ alongside acridine orange flow cytometry.
While the Comet assay exists‚ the others are favored. Crucially‚ the 6th Edition emphasizes that standardized thresholds are currently lacking; each laboratory must establish its own reference range using appropriate controls to ensure accurate interpretation of SDF results presented in the PDF report.
TUNEL Assay
The TUNEL assay‚ frequently detailed within a normal sperm analysis report PDF‚ is a method used to detect DNA fragmentation in sperm. It identifies DNA strand breaks by labeling DNA fragments with modified nucleotides. This assay is considered a valuable tool for assessing sperm quality and its potential impact on fertilization and embryo development.
The 6th Edition of semen analysis guidelines recognizes the TUNEL assay as a clinically useful test for SDF. However‚ it’s crucial to remember that the report’s PDF will reflect laboratory-specific reference ranges‚ as universal thresholds haven’t been established. Accurate interpretation requires comparing results to the lab’s defined controls and normal values.
Sperm Chromatin Dispersion Assay
The Sperm Chromatin Dispersion (SCD) assay‚ often documented within a comprehensive sperm analysis report PDF‚ evaluates the integrity of sperm DNA by assessing the dispersion of DNA fragments after alkaline denaturation; A tighter dispersion indicates increased DNA fragmentation‚ potentially hindering fertilization and embryo development.
Recognized by the 6th Edition as a useful clinical test for SDF‚ the SCD assay provides insights into chromatin packaging. However‚ like other SDF tests‚ a normal sperm analysis report PDF will present laboratory-specific reference ranges. The report emphasizes that each lab must establish its own controls for accurate interpretation‚ as standardized thresholds are currently unavailable.
Reactive Oxygen Species (ROS) Levels

Reactive Oxygen Species (ROS) assessment‚ increasingly included in detailed sperm analysis report PDFs‚ measures oxidative stress levels within the semen sample. While some ROS are necessary for sperm function‚ excessive levels can damage sperm DNA‚ impacting motility and fertilization capacity.
The 6th Edition acknowledges ROS as a significant factor in male infertility. A comprehensive PDF report may detail ROS levels alongside other parameters. However‚ interpreting ROS results requires careful consideration‚ as optimal levels vary. Laboratories are encouraged to establish their own reference ranges‚ as standardized thresholds remain undefined‚ ensuring accurate assessment of sperm health documented in the report.
Interpreting the Results & Reference Ranges

Semen analysis PDF results require careful interpretation; the 5th centile is a guide‚ but laboratory-specific reference ranges are vital for accurate assessment.
Age-Related Changes in Semen Parameters
Semen analysis PDF reports increasingly acknowledge age-related declines in male fertility parameters. Studies analyzing extensive datasets reveal significant trends with advancing age. Specifically‚ a notable decrease in both seminal volume and sperm concentration is observed. Research indicates the mean seminal volume decreased from 3.79 ml to 3.42 ml‚ while the mean sperm count declined substantially from 125.4 million/ml to 78.0 million/ml.
Furthermore‚ morphological abnormalities‚ such as an increased proportion of double sperm heads‚ also become more prevalent with age‚ rising from 0.52% to 1.51%. These changes highlight the importance of considering age when interpreting a sperm analysis PDF and assessing potential male factor infertility; Therefore‚ age-specific reference ranges are becoming increasingly relevant.
The 5th Centile and Normal Values
Interpreting a sperm analysis PDF often involves comparing results to established reference ranges‚ with the 5th centile being a key benchmark. The 6th Edition emphasizes that utilizing the 5th centile values for basic semen parameters is one method of interpretation‚ not the sole determinant of fertility potential.
Values falling below the 5th centile are generally considered abnormal and may suggest possible male factor infertility‚ prompting further investigation. However‚ it’s crucial to remember that normal values can vary between laboratories. A sperm analysis PDF should always include laboratory-specific reference ranges for accurate assessment. Abnormal findings necessitate referral to a male reproductive specialist for comprehensive evaluation and appropriate therapeutic intervention.
Accessing and Understanding a PDF Report
Semen analysis PDF reports contain vital data; understanding common sections and laboratory-specific reference ranges is essential for accurate interpretation of results.
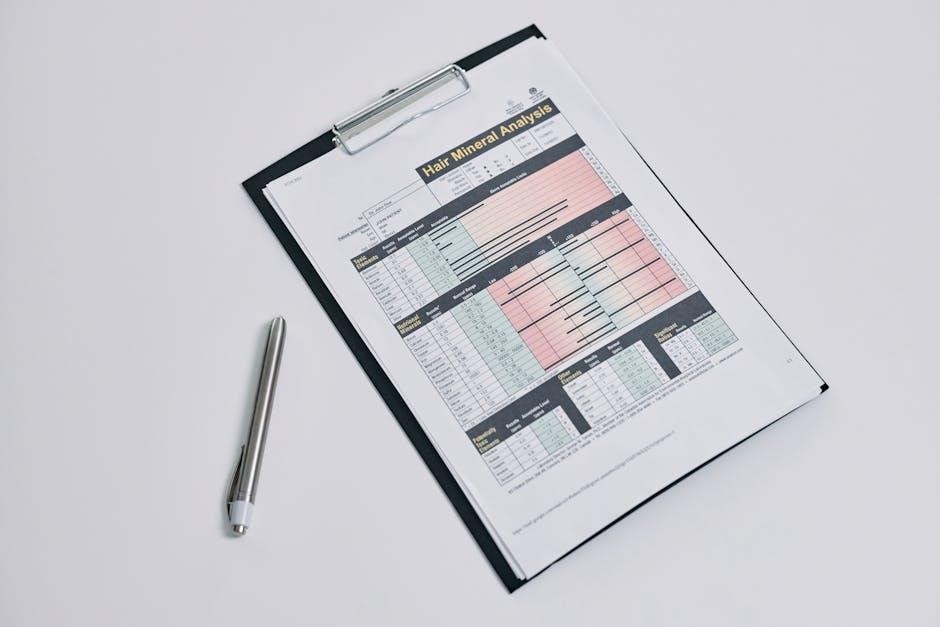
Common Sections of a Sperm Analysis PDF
A typical sperm analysis PDF report is meticulously structured‚ beginning with patient demographics and date of collection. Core sections detail fundamental parameters: semen volume‚ sperm concentration (count)‚ total sperm number‚ motility (progressive and non-progressive)‚ and morphology (assessing normal and abnormal forms).
Increasingly‚ reports include advanced tests like Sperm DNA Fragmentation (SDF)‚ utilizing methods such as the TUNEL assay or sperm chromatin dispersion assay. Reactive Oxygen Species (ROS) levels might also be present.
Crucially‚ each lab provides its own reference ranges‚ often based on the 5th centile‚ alongside results. The report will usually include notes regarding the methodology used and any observed abnormalities‚ guiding further clinical evaluation.
Importance of Laboratory-Specific Reference Ranges
Semen analysis results are heavily reliant on laboratory-specific reference ranges‚ as methodologies and population demographics can vary significantly. The 6th Edition emphasizes that standardized thresholds aren’t universally applicable; each lab must establish its own norms using appropriate controls.
Relying on generalized values can lead to misinterpretation‚ potentially causing unnecessary anxiety or delayed treatment. Factors like age influence these ranges‚ with studies showing a decline in seminal volume and sperm count with age.
Understanding a lab’s specific 5th centile values is vital for accurate assessment‚ as these define the lower limit of normal for that facility. Proper interpretation necessitates comparing results to these individualized benchmarks.